metastatic colon cancer to liver
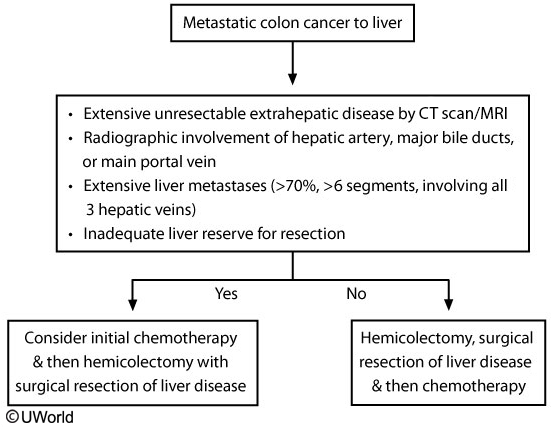
Approximately 20% of patients with colorectal cancer have metastatic disease at diagnosis. Common sites include the liver, lung, peritoneum, and lymph nodes. Most cases are incurable, but patients with liver-isolated colorectal cancer can sometimes be cured with surgical resection. Surgery can generally proceed if <70% of the liver is involved and there is no evidence of hepatic artery, major bile duct, main portal vein, or celiac/para-aortic lymph node disease. Subsequent chemotherapy should then be offered to maximize cure rates (~30%) and 5-year survival (~50%).
Lung lesions and metachronous liver metastasis (found after colorectal surgery) are also typically resected with curative intent. This patient with 2 liver lesions in a single lobe, a small primary tumor, and no other significant comorbidities is likely a good candidate for concurrent colorectal and hepatic resection followed by chemotherapy. After treatment, all colorectal cancer patients require regular follow-up with carcinoembryonic antigen testing, colonoscopy, and abdominal imaging to monitor for disease recurrence.
Chemotherapy followed by surgical assessment is used for those who do not initially qualify for concurrent surgical resection due to tumor invasiveness (eg, >70% of liver, portal vein involvement). For those with resectable hepatic lesions (as in this patient), surgery should be performed prior to chemotherapy due to the risk of chemotherapy-induced hepatic damage (eg, steatosis), which can limit the ability to operate.
Most hepatic metastases are diagnosed by noninvasive imaging and serum tumor markers. Hepatic biopsy adds little to overall diagnostic information and may reduce long-term survival.